As discussed in the Lancet Global Health Commission on Global Eye Health, screening for diabetic retinopathy depends on close partnership with general medical services to identify people with diabetes. Delivery of diabetic retinopathy screening is being transformed by increasing availability of lower-cost retinal cameras operated by non-specialists, acquiring images for remote grading.
In high-income countries, established diabetic retinopathy screening and treatment programmes deploy technicians to community settings to collect images for remote grading and referral decision. In the UK, for example, the proportion of blindness in the working-age population caused by DR has declined, due to both improved diabetes control and the national DR screening programme (Liew et al., 2014).
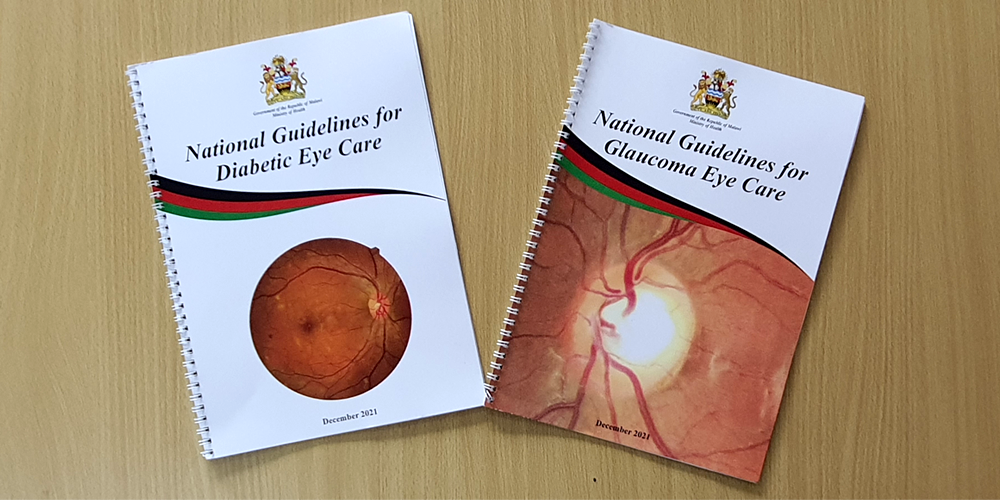
Programmes are also being developed in low- and middle-income settings. For example, in India multiple pilot programmes have been developed in the public health system under the Ministry of Health, demonstrating substantial increases in people screened at NCD clinics and community health centres (Murthy et al, 2020). In Sub-Saharan Africa and the Caribbean multiple countries have developed regional or national DR screening programmes following similar patterns of embedding DR service within general NCD clinical services (Poore et al., 2015).